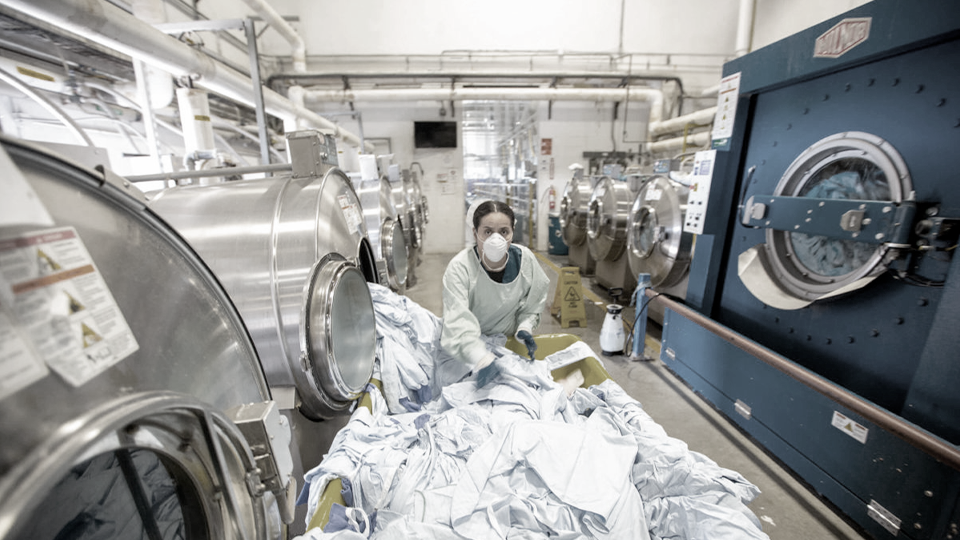
Decontamination of textiles is an enormous challenge in the healthcare industry. Due to its broad diversity, which includes bed sheets, towels, personal clothing, patient apparel, uniforms, gowns, and drapes for surgical procedures, it demands treatment that covers both: antimicrobial efficiency and will not be destructive to the fabric itself. How to make it sustainable and efficient?
How Important IS IT?
While contaminated textiles can be a source of vast numbers of pathogens, the literature reports of healthcare-associated diseases linked to contaminated fabrics are few in number. This observation leads to the assumption of the negligible risk of disease transmission during the laundry process. This is a major omission, as a simple calculation says otherwise. If we realize the amount of laundry made in healthcare facilities (estimated to be 2.3 billion kg annually in the United States) the risk becomes quite obvious. The emphasis should be put on continuous improvement of the process to minimize the risk of microorganism transmission, as well as for making the guidelines and procedures more sustainable.

Make it green
Indeed, the reduction of energy consumption recently became a key objective when improving the sustainability of cleaning operations. But not only: water use for textile treatment is also an important factor. Another issue will be the use of chemicals and detergents that will not harm the environment. All together has one goal: protection of the environment and reduction of CO2 emission. The ways of simple and effective ways for laundry cleaning and disinfection are: choosing the right product and procedures at lower temperatures.

The ideal solution?
The market delivers a broad choice of products designed for healthcare laundry. However, the selection of the correct formulation is complex. Most importantly, we should consider reducing the risk of the need to repeat the procedure due to insufficient cleaning. The ideal product will therefore prevent additional water heating, and electrical equipment running costs, producing savings in time and product consumption.
Decrease the temperature
The heating of water to an accurate temperature takes time and generates considerable cost. However, there are solutions developed to be effective at lower temperatures. These alternative products are proved to be as powerful as the traditional, well-known detergents. Moreover, formulations dedicated to laundry disinfection at lower temperatures can save around 35% on water heating costs, consume 34% less water and cut wash time by almost 20%. All these properties are nothing more than excellent sustainability gains.
Be effective
Look for standards and norms when it comes to efficiency. EN standards can be a great indicator. The minimum requirements are bactericidal activity (EN 13727 (2/1, dirty conditions), EN 16616 (2/2)) and yeasticidal activity (EN 13624 (2/1, dirty conditions), EN 16616 (2/2)). However additional standards provided by Robert Koch Institute (RKI) are also relevant. Most of the healthcare-delivered contaminated laundry will be ironed. That means that temperature will also have an impact on the survival of the pathogen.

Bibliography
- Rutala WA, Weber DJ. Uses of inorganic hypochlorite (bleach) in health-care facilities. Clin Microbiol Rev 1997;10:597–610.
- Mallison GF. Central services and linens and laundry. In: Bennett JV, Brachman PS, eds. Hospital infections. Boston, MA: Little, Brown, & Co, 1986;251–6.
- Blaser MJ, Smith PE, Cody HJ, Wang W-LL, LaForce FM. Killing of fabric-associated bacteria in hospital laundry by low-temperature washing. J Infect Dis 1984;149:48–57.
- (353) Barrie D, Hoffman PN, Wilson JA, Kramer JM. Contamination of hospital linen by Bacillus cereus. Epidemiol Infect 1994;113:297–306.
- Standaert SM, Hutcheson RH, Schaffner W. Nosocomial transmission of Salmonella gastroenteritis to laundry workers in a nursing home. Infect Control Hosp Epidemiol 1994;15:22–6.
- Association for the Advancement of Medical Instrumentation. Processing of reusable surgical textiles for use in health care facilities: ANSI/AAMI recommended practice ST65. Arlington, VA: Association for the Advancement of Medical Instrumentation, 2000;16



